Testing and Diagnosis
All porphyria diagnoses are confirmed by biochemical testing. “Clinical diagnoses” without positive biochemical results are not considered diagnostic of porphyria.
First-Line Testing
Screening tests (i.e. first line testing) are not the same for all porphyrias. Testing must be tailored to the presenting symptoms and the type of porphyria suspected.
An acute hepatic porphyria (AHP) should be suspected if a patient presents with neurovisceral signs and symptoms and an initial evaluation excludes more common causes. With the very rare exception of ADP porphyria, PBG is expected to be substantially increased in all patients during acute attacks but not in other medical conditions.
Tests
Spot urine porphobilinogen (PBG)
Urine total porphyrins
These tests can be done properly at any laboratory. See Random Urine Testing Reference Guide for AHP for details on test codes and specimen collection for major U.S. laboratories.
Testing Notes
Urine PBG is generally not included in urine total porphyrin tests. Concentrations of PBG in the urine depend in part upon how dilute the urine is, they are best expressed normalized to urinary creatinine concentrations [mg PBG/ g creat or mmol PBG/mol creatinine]. This test is both sensitive and specific.
Obtain sample when symptoms are present, if possible
Samples are sensitive to light and temperature. Samples should be collected in brown containers or wrapped in foil after collection, shipped with dry ice and stored in a fridge or freezer.
Measurement of total urine porphyrins is recommended even though porphyrin elevation is nonspecific, because porphyrins may remain increased longer than PBG in AHPs (especially in HCP and VP). Urgent first line measurement of ALA is not essential, because ALA elevation from ADP or any other cause is always accompanied by increased porphyrins.
Interpretation and Next Steps
Normal urine PBG and total porphyrins essentially rules out an AHP as the cause of concurrent symptoms. However, slight elevations of PBG and porphyrins may not support a diagnosis of AHP, especially with more sensitive methods that result in a narrow reference range.
When marked elevation in PBG establishes a diagnosis of AHP, more extensive second line biochemical and/or genetic testing should be done to differentiate these conditions.
Elevation in urine porphyrins without elevation in PBG also requires further evaluation by second line testing, to include urine ALA and plasma and fecal porphyrins, which if normal will exclude ADP, HCP and VP.
Tests
Plasma total porphyrins
Urine total porphyrins
These tests can be done properly at any laboratory. See Random Urine Testing Reference Guide for AHP for details on test codes and specimen collection for major U.S. laboratories.
Testing Notes
Samples are sensitive to light and temperature. Samples should be collected in brown containers or wrapped in foil after collection, shipped with dry ice and stored in a fridge or freezer.
Interpretation and Next Steps
Normal results effectively excludes cutaneous porphyrias.
Further second line testing is needed if porphyrins are increased, because these findings are not specific, and porphyrinuria (especially coproporphyrinuria) is common in other diseases. If second line testing is negative, then porphyria is not present.
Tests
Erythrocyte protoporphyrin
Plasma total porphyrins
At present, only the UTMB Porphyria Lab and Mayo Medical Laboratories are recommended for these tests
Testing Notes
Samples are sensitive to light and temperature. Samples should be collected in brown containers or wrapped in foil after collection, shipped with dry ice and stored in a fridge or freezer.
Interpretation and Next Steps
Normal results excludes non-blistering cutaneous porphyrias.
Genetic testing is required to differentiate between EPP and XLP.
Table 1. Laboratory Findings in the Non-Blistering Cutaneous Porphyrias
Second-Line Biochemical Testing
When marked elevation in PBG establishes a diagnosis of AHP, more extensive second line biochemical and/or genetic testing should be done to differentiate these conditions.
Labs that can be used for second-line testing include: UTMB, ARUP, Mayo, Quest, and LabCorp.
Additional Tests
Urine ALA
Fecal Porphyrins
Plasma Porphyrins
Testing Notes
Obtain sample when symptoms are present, if possible
Samples are sensitive to light and temperature. Samples should be collected in brown containers or wrapped in foil after collection, shipped with dry ice and stored in a fridge or freezer.
Table 2. Second-line Biochemical Testing for AHPs: Laboratory Findings to Differentiate the four Acute Hepatic Porphyrias
Elevation in urine porphyrins without elevation in PBG requires further evaluation by second line testing, to include urine ALA and plasma and fecal porphyrins, which if normal will exclude ADP, HCP and VP.
Labs that can be used for second-line testing include: UTMB, ARUP, Mayo, Quest, and LabCorp.
Additional Tests
Urine ALA
Fecal Porphyrins
Plasma Porphyrins
Testing Notes
Obtain sample when symptoms are present, if possible
Samples are sensitive to light and temperature. Samples should be collected in brown containers or wrapped in foil after collection, shipped with dry ice and stored in a fridge or freezer.
Interpretation
See Table 2
Elevation of urine coproporphyrin only is not diagnostic, because it occurs in a number of other medical conditions, notably in heavy users of alcohol and/or liver disease. Elevation of ALA and coproporphyrin (with normal PBG) is typical of lead poisoning, which should be confirmed with a blood test for heavy metals (lead, mercury, arsenic).
Table 2. Second-line Biochemical Testing for AHPs: Laboratory Findings to Differentiate the four Acute Hepatic Porphyrias
Total plasma or urine porphyrins are measured when porphyrias are considered as a possible cause of blistering skin photosensitivity. Normal results effectively exclude these cutaneous porphyrias. Further second line testing is needed if porphyrins are increased, because this finding is not specific, and porphyrinuria (especially coproporphyrinuria) is common in other diseases. If second line testing is negative, then porphyria is not present.
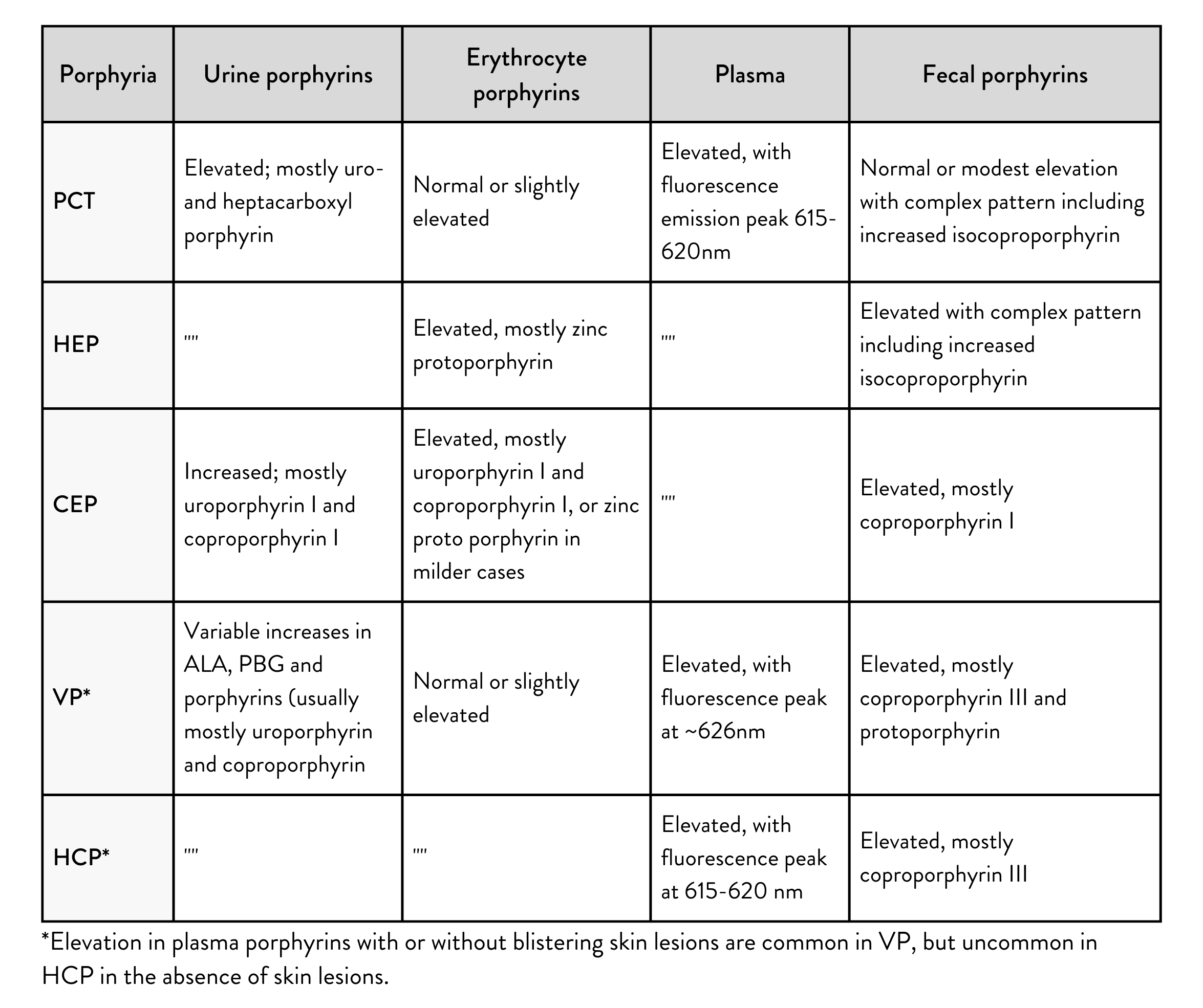
Table 3. Laboratory Findings to Differentiate Blistering Cutaneous Porphyrias
Genetic Testing
Confirmation of the diagnosis by genetic testing is recommended for all porphyrias. Importantly, knowing the familial mutation(s) enables screening of family members who may be at risk for developing symptoms or may pass a pathogenic mutation to the next generation. If the type of porphyria has been proven biochemically, it is usually necessary to examine only one gene to identify the responsible mutation. Once the familial mutation is known, the testing of family members can be targeted to that mutation.
Table 4. Genes Responsible for the Porphyrias