Meet Claudia, VP Warrior
By Claudia
"As I tried to call emergency services, my legs gave out. Then my arms grew weaker—I couldn’t hold the phone."
-Claudia, VP patient.
My name is Claudia, I am 49 years old, I come from Germany and I have 2 rare diseases: Porphyria (Variegate Porphyria) and Hypokalemic Periodic Paralysis.
01.07.2023: I had breakfast and suddenly felt such a weakness that I just managed to go into the living room and lie down on the sofa. I was afraid of being paralyzed again. Today of all days I was alone in the house. My husband and my son were on the road, my mother was on vacation and I couldn't reach my best friend either. Luckily, I had my phone with me, because I suddenly realized that I couldn't move my legs anymore. My arms were also getting weaker and weaker and I could barely dial the emergency number. Then the phone slipped out of my hand, because now my arms were also paralyzed. The phone was now next to me on the sofa. It rang: probably my friend calling back. I couldn't answer it and tears rolled down my face.
The paramedics were there within 10 minutes. Patient paralyzed from one moment to the next, they didn't have that yet. Luckily, after another 10 minutes my best friend arrived: she’d been worried when I didn’t answer my phone, as she knew I had been feeling unwell for days. She accompanied me in the ambulance.
I knew about my Porphyria for some months now and because my legs were paralyzed a week ago, after a detoxification infusion with my family doctor, I had already contacted my treating Porphyria specialist. However, he said that the weakness and paralysis could not come from Porphyria as my corresponding values were not high enough and such sudden paralysis was atypical.
So much went through my head: all the last 15 years I had struggled with health issues. I had pain all over my body. Unbearable back pain, flank pain, which tore me apart, especially at night from 03:00 a.m. onwards. Sleep was then out of the question. Then all these intolerances: I could hardly tolerate anything to eat, had fructose and histamine intolerance and many other food intolerances. I had a fragrance allergy, MCS (Multiple Chemical Sensitivity) and could not tolerate electrosmog. I was permanently weakened and could not be near metal, otherwise my pain worsened. I had severe skin problems, was constantly tired and didn't feel compatible with this world anymore. Summary: I couldn't tolerate anything to eat, couldn't be anywhere else and had constant pain!
In all these years, I had consulted countless doctors: family doctor, orthopedist, neurologist, neurosurgeon, rheumatologist, gynecologist, nephrologist, urologist, holistic doctors, orthodontists, surgeons, alternative practitioners, building biologists, physiotherapists, osteopaths, dermatologists, allergists, pain clinics, cures, Chinese medicine, psychotherapy, various hospital stays and much more.
Additionally, I had taken advantage of everything that was possible in terms of therapies, whether through health insurance or privately. I even had surgery on my back (denervation of the facet joints) because I couldn't stand the flanks and lumbar spine pain anymore. Unfortunately, it didn't help. Like most therapies. I couldn't tolerate any painkillers that were prescribed to me, which only made it worse and added heart problems and other things.
“Trapped in my own body, I could only listen as doctors and nurses talked about me like I wasn’t there.”
-Claudia, VP patient.
I had spent a lot of money on private doctors, alternative therapies and dietary supplements. Nothing went away, something was always added. My medical and hospital reports now filled 5 folders. Plus 2 more folders with self-made notes, internet printouts, etc. The list of my diagnoses became longer and longer.
And now I was in the ambulance again, this time paralyzed from my neck down. I just couldn’t take any more as I felt this was no longer a life. In the ambulance, I seriously asked my friend, if I remained paralyzed, to take me to Switzerland, where assisted dying is legal, so that I could take my own life.
In the last 2 years, I have been paralyzed several times from the neck down after dental treatments, back surgery and my eye surgery. In the hospital, I was treated so terribly that I then researched what it could be. That's how I came across Porphyria, and suddenly had to cry bitterly watching a patient video. I've never had that before! At that moment I was one hundred percent sure that I had this disease, it just had to be diagnosed. So I found a laboratory through my health insurance company that specializes in Porphyria. The examination of blood, urine and stool has revealed the variant Variegate Porphyria. Later, this was also genetically confirmed (PPOX gene). Porphyria can lead to paralysis, but this should probably not be the (only) reason for me.
The local hospital, where I was now admitted, then contacted my Porphyria doctor. He said that the paralysis could not be because of Porphyria, because it came too suddenly and the values were not high enough, but so that I did not actually slip into a flare-up, I should get glucose infusions. The glucose infusion then made me actually be able to move again! However, as soon as the infusion had gone through, after 5 minutes I was paralyzed again from the neck down. I was administered a pain relief injection for my severe back pain, which resulted in additional unable to open my eyes or speak. All I could do was hear and breathe. Nothing more. It was cruel! To make matters worse, the doctors and nursing staff in my room were talking about me as if I wasn't there! I could have burst inside. After a few hours, I could at least speak again, but I was still paralyzed from the neck down. I asked the nurse for a drink, who brought me a sippy cup of water and put it on the bedside table. It was just unbelievable! She knew exactly that I couldn't move. I told her that I couldn't get to it. So she put the sippy cup on my bed, looked at me annoyed and went out without saying anything. I had the water right next to me and couldn't get to it. How cruel that was! I have never experienced anything so terrible. And I was so thirsty! I hadn't drunk anything for hours.
Occasionally I received another glucose infusion and was able to move a bit again after some time. It was very clear to me: I had to get out of this hospital! I won't survive here. However, they didn't want to issue me a transport ticket to another hospital, after all, in their opinion, I didn't have anything. As soon as I was able to grab my phone again, I arranged an ambulance myself, which wanted to take me to the university hospital on the same day. I would have self-fund this at a cost of 3000 €, but I didn’t care. I just wanted to discuss it with my husband, when I had to see with horror that my glucose infusion was still running only for maybe 5 minutes. And then I was paralyzed again. For hours. And that day was over, too.
“The medical team clearly suspected I was faking; how else could they explain my sudden paralysis when MRIs and spinal fluid tests showed nothing?”
-Claudia, VP patient.
I was sure it was a Porphyria flare-up and wanted to prove it. I wanted to have my urine sent to the special laboratory, but the doctors didn't give me permission. So I wanted to send my urine there myself later (as I had a catheter and could therefore manage this), but I was forbidden to do that as well. I just thought: “Now they're all crazy here, I can send my urine wherever I want and have it examined at my own cost for whatever I want!” I needed the proof, because I was sure that I needed hemin, which was not known here (For Periodic Paralysis patients: hemin is an infusion for the treatment of acute Porphyria flare-ups).
I was in this hospital for a week. It was an up and down between full-body paralysis and being able to move, depending on whether I got a glucose infusion or not. The doctors and nurses probably actually thought I faked it, as it is actually hard for an outsider to believe. An MRI of the head was done and a cerebrospinal fluid examination. Both were inconspicuous. After a week, they wanted to send me to a psychiatric clinic. However, I definitely didn't see myself there and disagreed.
So they had me brought home in a patient-transport and put me to bed paralyzed. It was so awful! My husband was completely desperate and my family didn't know what to do either. So I lay in my bed at home, still catheterized, whilst my family took turns staying with me.
We then talked to a doctor from the health insurance company, who recommended a university clinic to us. 2 days later, in a moment when I was just able to move a bit, my husband gathered all his courage and then took me there. What if I get paralyzed on the highway? Do we call the ambulance then? What if I experience breathing problems? What if the hospital doesn't accept us? After 2 hours of driving, I was actually completely paralyzed again and I was pulled out of the car by several people in front of the clinic and put into bed. From that moment I knew: now things are looking up, here I will be helped. I immediately got a glucose infusion and finally hemin. I was so grateful.
After another week in hospital with 24/7 glucose every day and hemin for 5 days, I was discharged and was finally no longer paralyzed. Weakened, It took weeks for me to get back on my feet. In the meantime, I got my Porphyria values: They were significantly elevated, more than 5 times the norm, but not as high as usually seen in patients with acute flare-ups of AIP. But, as I said, I have the rare variant Variegate Porphyria, which only exists a few times in Germany (5 to max. 10 people?). Later, a Whats-App group from South Africa, where the variant is more common, helped me a lot. Thank you, dear ones, if you are reading this! I also read case studies and registered in various porphyria Facebook groups. Again, thanks to all admins!
It seems that with the Variegate Porphyria the values are not as much increased during flare-ups as with the AIP. I also discussed this afterwards with my Porphyria specialist. In the meantime, a 5-fold increase is probably also seen as an acute attack, especially in VP patients.
When I was weak at home, I had always sucked glucose tablets at so that I didn't fall into paralysis again. A few weeks after the hospital stay, however, the time had come again.
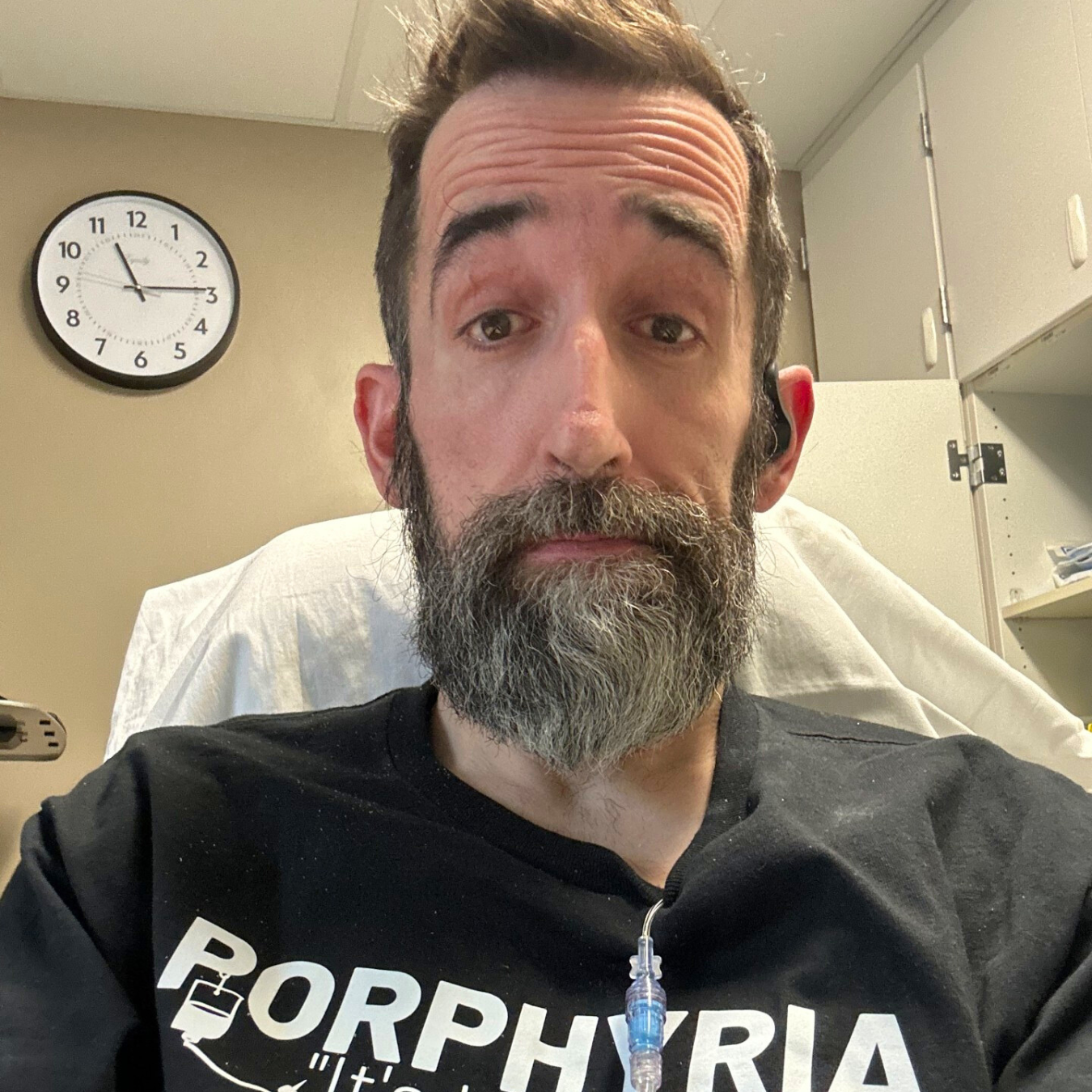
Claudia feeling good.
The weakness was so strong and I felt on the verge of paralysis again. Just don't call an ambulance, I thought, it will only take me to the local hospital, where I have now been treated several times impossible. So my husband took me back to the university hospital, which was 2 hours away. Again glucose, again hemin, after 1 week back home.
The doctor from the university clinic saw a severe case in me, so he prescribed me the medicine Givosiran (also a medicine for acute Porphyria patients). Unfortunately, the paralysis did not go away and I ended up more often in the university hospital. At some point, however, they stopped the glucose infusion and didn't want to give me any more hemin infusions, because they thought that I should no longer be paralyzed with the Givosiran treatment. Shortly after stopping the glucose infusion, I was paralyzed from the neck down again. And soon afterwards there were rounds. The doctors were frightened and quickly readministered the infusions. 4-5 doctors and the nursing staff stood in front of me and didn't know what to do. The words they said will remain in my memory forever: "Not that we missed anything!"
I made up my mind: as soon as I am discharged from the hospital, I will have my blood tested for all minerals, vitamins, trace elements and amino acids that can be tested in the laboratory. Something had to be missing! And I'm going to keep researching on the internet until I find what I have! If you, dear doctors, don’t find it, I'll find it out for myself.
Back home, I had my blood thoroughly tested, directly in the laboratory. It was hard to believe: my blood values were great, only my potassium value was too low. I had heard this several times over the years and have therefore been prescribed potassium capsules several times. Still looking for another cause, I googled "potassium deficiency" and "paralysis" and came across Hypokalemic Periodic Paralysis on the internet. I didn't find much on the German pages, so I came across the Periodic Paralysis Association from America. There were fantastic patient reports (thanks to you!), where I felt absolutely addressed again. Especially in a video where the patient was pulled paralyzed out of the car in front of the clinic. Just like they did with me. It shivered down my spine. I had found it! I also watched all of Dr. Cannon's lectures. Now I knew the genes that needed to be examined and found a laboratory in Germany that examined them. Once again, I paid for it myself, because it would have taken too long to go through the health insurance and I was finally tired of discussing diagnostics with the doctors! Then I only heard, as with Porphyria: “This is so rare, you can't have it!”
I could have bet that I had the Hyper version of Periodic Paralysis (HyperPP) since I got out of paralysis on glucose. However, Hypokalemic Periodic Paralysis (HypoPP) had been confirmed (CACNA1S gene). Which probably explains why I was paralyzed again immediately after the glucose infusion, worse than before. And the whole thing had escalated so much due to the many glucose infusions and tablets that I was now paralyzed weekly.
I discussed my new diagnosis with my attending physician. He then prescribed me spironolactone (a medicine, which is prescribed in Germany for Periodic Paralasys patients) – and poof, I had another attack. Again university hospital. When I registered, I presented my new diagnosis and asked to be able to lie down immediately. I was so weak! No, that wouldn't work, I'd see what's going on here! Oh yes, I saw it. There were about 50 patients in front of me, each with accompaniment, and correspondingly loud. This was the last shock I needed to fall into paralysis. I sat on the registration chair and couldn't move an inch. My blood pressure was 150 to 100 (usually 110/70) and I felt like I couldn't breathe. Tears rolled down my cheeks. They immediately called my husband, got a bed, put me in there and pushed me straight to the doctor. At least I got my turn right away... During this hospital stay, however, I realized that no one knew about the rare desease Periodic Paralysis. I was the one who informed the doctors about the disease. Patient informs doctor about rare disease. So I had to take care of myself again as soon as I was home. And I signed up for the Facebook group "PPSN – Periodic Paralysis Support Network".
“ Never give up! We keep going! Solutions will come!”
I just say: thank you, thank you, thank you to all the fellow patients who shared their experiences here. And thanks to Ralph for leading this group so fantastically! So I came to the conclusion that I can get out of the paralysis within 20 minutes with potassium bicarbonate. It must be fast acting, not slow release potassium. No doctor could have given me that tip. It just has to be given to me by someone with a sippy cup – after all, I can't move anymore... Since I can no longer reach my phone, at some point I had the idea to use the SIRI function of my cell phone to call my husband, who then comes and gives me potassium. When I'm slurred on the phone, he already knows. Thanks to my husband and to the technology.
And I got to know my triggers, I wrote down all the triggers that other patients reported about in the Facebook chats. I kept a diary and wrote down for many months what I ate, drank, did and when I was weakened or even paralyzed. I have found out many triggers and can avoid them. But some I can’t: for example, hormones. Always at the end of my period I was totally weakened for 3 days and completely paralyzed once. The same applies to ovulation. Unfortunately, I still haven't found anything that suppresses the hormones in such a way that these paralysis do not occur. Sometimes I just can’t explain the weakness or the paralysis. You can't always find a reason.
In between, I also had an appointment at another university hospital, where a doctor is familiar with Periodic Pralysis. She prescribed me acetazolamide, which sadly only made it worse for me. I was no longer completely paralyzed, but I lay permanently weakened on the sofa for several weeks. That wasn't a solution either, so I stopped taking the medication again. Then it's better to be completely paralyzed every week but in between for a few days where it goes quite well. The drug is dichlorphenamide., which is available in America, is unfortunately not approved here in Germany. A fellow patient tried to apply to the health insurance company anyway - unsuccessfully. So I have to live with the weakness and paralysis.
Because of Porphyria, I have been getting a Givosiran injection for over a year and I can only say: thank you, thank you, thank you! Thank you for getting the medication and thanks to the nurse who gives it to me at home every 4 weeks. The medication didn't help against the paralysis, which is why I got it in the first place, but my nightly unbearable flank pain has completely gone away. And all my joint pain has gotten much better. The connection with all the (nerve) pain and porphyria has not been seen (or wanted to be seen), before.
Unfortunately, because of the HypoPP I am now paralyzed about 1 x a week and often so weakened that I can only stay on the sofa. And unfortunately, my intolerances and allergies have not disappeared either. But my body seems to calm down and we manage it well. Potassium in the sippy cup is my absolute emergency medicine. And there are always good days in between, which we then absolutely enjoy.
How does my husband always say so beautifully? "Never give up! It goes on and on! We will find a solution!" Thank you!
Best regards to all, Claudia.
Claudia’s journey with VP.
Want to share your story? Contact us at katri@porphyria.org