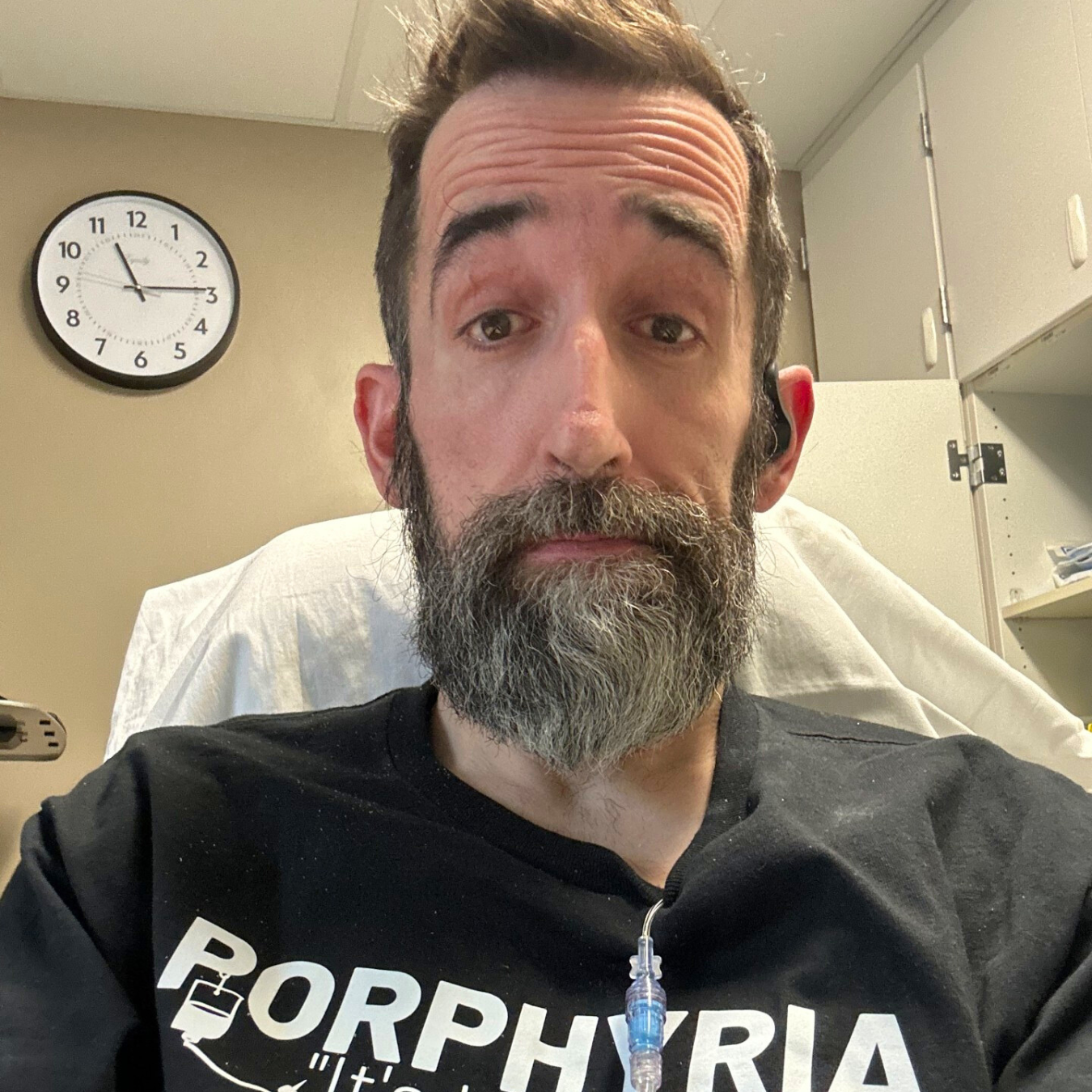
Meet Joni, VP Warrior
“I would have reoccurring, unexplained abdominal pain and headaches, always in the same place, fragile skin and seizure like reactions to most medications.”
Joni, VP patient.
As I look back on my life, my porphyria journey began in my 20’s when I started on birth control pills. I would have reoccurring, unexplained abdominal pain and headaches, always in the same place, fragile skin and seizure-like reactions to most medications. During my childbearing years, I had two miscarriages and one very serious tubular pregnancy that ended up in a ruptured fallopian tube and the surgical removal of that tube. After my miscarriages, I was always given a medication to shrink my uterus that resulted in more seizure-like activity. In those days, the doctor instructed me to “take a shot of brandy, take a hot shower and go to bed”. (I know now what a poor solution to the problem that was!) I have two beautiful boys to show for all my problems in childbearing.
As the years went on, I knew that I was “different” and that my body had a mind of its own, but I had no idea the extent of how different I really was. I almost always wore gloves when outside because the skin on my hands was so fragile that even a small bump would result in peeling back of the skin on the tops of my hands. My abdominal pain and nausea seemed to be because I didn’t eat regularly and I always craved carbs. I could out eat most men and have been fortunate enough to retain my “100 pounder” status through it all thanks to a metabolism similar to that of a hummingbird.
I was a professional violinist for over 30 years along with many other fascinating occupations to keep the “starving artist” afloat. Over the years more unexplainable symptoms appeared. I began to have muscle pain which I attributed to too much repetitive work. If I took Tylenol, I would soon end up in the hospital with unexplained seizure-like activity that would resolve in about 24 hours. Advil and Aspirin offered the same outcome. My muscle pain would come and go with different intensities. I had no tolerance for alcohol-one mixed drink and I was pretty much dysfunctional. A cup of coffee put me in a state of hyperactivity and gave me nausea, I was pretty much no fun!
Fast forward about 20 years to 2009. I was playing on the road about 27 weekends out of the year and many outdoor “gigs” in the summers, and I was also going through menopause. Hot-sunny-stressful. But, I was having the time of my life and felt that my career was at an apex when, all of a sudden, my body broke down. I could no longer even hold my violin up, I couldn’t sleep due to what I know now as nerve pain. I was having more recurrent abdominal pain and nausea and I was forced to quit all that I knew for all of my adult life.
“For the next two years I went through every muscle pain relieving treatment known to man: acupuncture, acupressure, PT, dry needling, massage, chiropractic, strain/counter strain, bio-feedback, hydrotherapy and rest.”
Joni, VP patient.
I went to my doctor with my symptoms and was diagnosed with Myofascial pain. Okay, what’s that? For the next two years I went through every muscle pain relieving treatment known to man: acupuncture, acupressure, PT, dry needling, massage, chiropractic, strain/counter strain, bio-feedback, hydrotherapy and rest. At one point, a steroid back injection was going to be performed after not finding a darned thing wrong with my back, I rapidly declined. Nothing worked. I continued to pursue my issues and went back to my doctor and he prescribed hormone therapy for my hot flashes, perhaps the muscle pain that I had and menopause in general.
While on hormones, I went to an outdoor weekend obligation. I had forgotten to wear gloves and my hands were totally covered in huge blisters. Near the end of the weekend, I remembered to put my gloves on but when I took them off at the end of the day, the skin on the entire top of my hand came off with the gloves! I went back to my doctor and he said he could only think of one thing and did some tests that revealed a diagnosis of Porphyria Cutanea Tarda (PCT). Okay, what’s that? My ferritin levels were above 1500 and so began my phlebotomies along with taking me off of the hormone therapy. Now, I was having phlebotomies to bring my ferritin levels back to around 150 and ongoing treatments for muscle pain and reoccurring abdominal pain. I tried to absorb as much information as I could to help justify all my troubles. I continued to also have an increase in unexplained “seizure-like activity” that came right out of the blue-no rhyme or reason. One day at PT, the therapist was dry needling many of my rock hard muscle knots and sent me on my merry way. I didn’t even get to the bottom of the stairs when I felt nauseous, faint and totally out of control. I ran back to the therapy room and commenced to have a full fledged seizure. After, I asked the therapist what just happened and she said she didn’t know, not very helpful.
Two years later in 2018, I was then sent to a neurologist who after many tests, diagnosed me with Stiff Person Syndrome (what Celine Dione has recently been diagnosed with) also known as SPS. Okay, what’s THAT??? I was put on valium and clonazepam for my sleep issues and muscle pain and began apheresis which is basically a plasma exchange therapy because in Stiff Person Syndrome, the problems lie in the plasma. My first port was put in. I continued my phlebotomies, PT, not sleeping and now the Apheresis. I was now having full blown seizures multiple times daily so the valium/clonazepam doses were steadily increased and so were my seizures. I began to lose weight and become extremely weak in my legs. One day, my husband and I went trout fishing, which we both love to do, and my legs became so weak that all I could do is sit down and cry. He thought I was overheated and tossed a cooler full of melted icy water over my head which only made me cry more. He carried me to the car and I recovered at home. At this point, I was so afraid of my body that I didn’t know what to do-things would just happen. Now, when I had my reoccurring nausea and abdominal pain, I added tachycardia and severe headaches to the mix. I was pretty much sure that I was about to die and prayed it would be swift. My seizures now also included uncontrollable crying, I had no idea why I was crying, I just was. I could talk and kept repeating that I didn’t know why I was crying. These seizures lasted about 45 minutes to an hour.
Photo of an eagle taken by Joni.
In late 2018, my ferritin levels held below 150 and I was able to stop the phlebotomies but was instructed all the good things about the sun and I took it very seriously but, all my other symptoms had increased to the point that I was riding the handicapped cart at the grocery store and a wheelchair at the clinic, wasn’t sleeping and became ill all over. I was hospitalized several times for my now called “tremors”, nausea, severe headaches and abdominal pain, but always released the next day with a pat on the head that sent me back to my Apheresis treatments.
In early 2019, I received a letter from the Neurology department from the PA that was working with my neurologist saying that she didn’t think that I had SPS and that the apheresis was going to be discontinued. I haven’t explained this, but on the medications that I was on, I had become an extremely volatile person and with this news, I absolutely blew a fuse. Now down to 80lbs, I physically wheeled into our clinic, demanded to see my doctor, slapped the letter on his desk and said, in not very nice words, that I needed an explanation. He stuttered and said that his PA came from a different background and he still felt that I had SPS. My drug induced bad personality said that I didn’t believe him and that I wanted a second opinion and I wanted it now. (Needless to say, it’s the last time he and I crossed paths-I have broken a few bridges along the way with my clinic but I was not going in the right direction and was absolutely scared to death).
In April of 2019 hovering at 80lbs with a BMI of 15, I wheeled into a large world-renowned hospital to undergo extensive testing for my issues. The first thing was to get me off the medications. Ok, that’s no problem, I just quit. Many tests were done and 5 days later I absolutely hit a wall: I couldn’t eat, couldn’t sleep, was agitated and miserable. “Maybe I should take those meds again just to see if they help?” When I did, I immediately felt better. OMG!!!!!! IM ADDICTED!!!!!! So, I went off again and like clockwork on day 5, I hit the same wall that I hit the first time. I read up on addiction to valium/clonazepam and tried the slow approach for a week-day 5-BAM. So, I did it over 2 weeks-day 5 BAM. I was still having extensive testing while this is going on and I just stayed off the meds and hoped that I would life through it all.
I went to all the different doctors. Neurology confirmed that I did not have SPS (well that’s a relief!). Psychology said I had anxiety which was why I have tachycardia. The Pain Center said that I had fibromyalgia because I had all the pain places. GI said there’s nothing wrong with your gut and there’s no explanation for all of the abdominal pain. Dermatology said that I had a very weird skin condition, I don’t remember what it was called, recommended a topical medication that had amitriptyline and ketamine in it, which I immediately had a seizure from, and promptly stopped using it. Finally, the last office that I visited was Genetics who discovered my PPOX mutation and told me that I had Variegate Porphyria and acquired PCT.
Photo of a wolf taken by Joni.
In August, my testing was completed, my diagnosis confirmed and I was sent back to my little clinic who had no clue as to what to do with me now. I was told that I just had to live with the pain and there wasn’t anything else that they could do for me: in other words, TOUGHEN UP BUTTERCUP! My symptoms escalated but my seizures subsided a bit. I began to slowly put on weight and walk a bit more but was incredibly weak. One night, I had the worst porphyria attack ever: seizures that wouldn’t stop, excruciating headache, body pain, nausea and that oh so familiar abdominal pain . After 6 days in the hospital, I was finally introduced to hemin and I would love to say that my story ends there, but it doesn’t.
First I had a PICC line put in place and I had severe reactions to the tape that kept the site closed to infection. After a week a regular port was implemented and I started my hemin journey. I had many of the usual problems with hemin: I couldn’t get it regularly, they didn’t know how to mix it, on and on but I did manage to get regular treatments. Recovery was slow but I felt the improvement. My skin around the port site was becoming very degraded from the blisters from not only the tape but the Betadine scrub also. That port was removed and another one put in on the other side. I was starving for answers to my symptoms. My diagnosis was confirmed but perhaps not the PCT?
After about a year and a half, my doctor said he didn’t think I was improving enough with hemin and thought it would be good to take a break from the treatments. In reality, he was tired of my problems with the tapes around the port insertion site. We tried every adhesive known to the medical world and I continued to have quarter sized (and larger) blisters around the site that absolutely drove me crazy with discomfort. I agreed to take a break from the treatments and the port was removed but not without a bang. During the procedure, the attending nurse, who was a good friend of mine, asked me how I was doing. Well, now that she mentioned it, not too well. I felt a seizure coming on and it let loose during the removal. I had warned the Dr. that I had no idea if I would react to the medications or not and I distinctly remember him saying “I’ve never done this on a moving target”. Not reassuring but humorous just that same. After the procedure and my 45 minute seizure, I asked my friend, the nurse, why at that particular time did she ask my about how I felt. She said “because your blood pressure took off and about hit the roof”. Well ok then, lets add “high blood pressure” to the list of symptoms, shall we?
Since my release from hemin, I have taken it upon myself to be very informed about the current information available about porphyria and did an in-depth research in my particular PPOX mutation. I wanted to inform my relatives about my VP for their information but didn’t know exactly which parent this came from. You see, they said that because of my Dad’s genetic Dutch heritage, it was assumed that I received this blessing from him. What I haven’t explained is that my sister inherited another rare disease from our Dad- Waldenstrom’s Syndrome. Unfortunately she passed away early from complications from this disease. In my research, I figured that it wasn’t very probable that two siblings received two different gene mutations from the same parent, it just didn’t make sense. My local doctor helped me obtain porphyria study papers that I found online and low and behold, there is a “founder effect” in Poland and my particular mutation was one listed. My mom had Polish blood, BINGO! So, now I knew which side of the family to contact with my information in case they wanted to pursue porphyria testing for themselves. I’m happy to say that no relatives have tested positive for VP. I have informed them as much as I can and if there are problems, they know where to look.
Joni’s photography.
My story took a marvelous turn at about the time I was at my lowest in 2019. I had no purpose in life, I felt ill and I was truly very depressed. What was I good for? What was I going to do with the rest of my life? My oldest son called me one day to see how I was doing and said he was going to get a new camera and asked if I would like his old one. Well, I said I didn’t know how I could take pictures if I could hardly walk, but sure, he could send it. This is a long and beautiful segue from despair to a new life.
As an artist and artistic person, I’ve always had three things that were always a passion for me: music, nature and animals. When I received his camera I began to heal emotionally with tying all three of those things into Nature photography. Today, I have a small photography business that I call The Variegate Lens Fine Art Nature Photography. I carry my wrist bands around every lens that says that “I’m a Porphyria Warrior” and will share my story with anyone who asks. I don’t wear my disease on my sleeve, I wear it on my camera equipment.
The word Variegate can also be tied to nature with all the different textures, colors and sounds, so depending on which story you want to hear, I have two. I now have a website, sell stock photos through Adobe, attend several art fairs in my area along with having my art in different art galleries. I submitted several years in a row to the NORD art contest and, although I never won anything, it did help to spread the word about porphyria to the rare disease community.
I now have purpose. I can fulfill my passions and have learned my limitations along the way. I am no longer afraid of my body, I’ve learned to have a great deal of respect for it and compassion for what I’ve been through and I feel like a true warrior. After 10 years of trying to find answers, I have Variegate Porphyria, I have pain, I have food and drug intolerances, I am centrally sensitized and I struggle with sleep issues, but I am also a survivor. I cook all my food from whole foods and don’t eat out, and I’ve learned to say “no”.
I just had a milestone last year as I went 12 months without a porphyria attack in 50 years, I am now 71 years old. I have liver ultra sounds twice a year and annual testing to make sure my porphyria is under control. I am my own advocate and bring new and important information to my doctor and we now work together. Although I’ve had some rough interactions along the way, I firmly believe that they respect my knowledge of my disease. I will continue to bring porphyria along with me on my life’s journey, but it no longer is in the driver seat.
My advice to others is to stay strong, stay the course, trust your own intuition and learn all that there is to learn about your type of porphyria. Remember to keep up with all the current information that is constantly being studied. Be a participant in porphyria studies if you can, it only helps others who are struggling.
Joni’s story with VP.
Want to share your story? Contact us at katri@porphyria.org