Meet Savanna, AIP Warrior
By Katrina Parra
"I was overcome by relentless abdominal pain, vomiting, and an inability to keep anything down."
-Savanna, AIP patient.
Savanna’s story with Acute Intermittent Porphyria (AIP) began at 18, a time typically marked by newfound freedom. With a strong family history of porphyria, she entered adulthood aware of the possibility but living in uncertainty. Warnings about specific triggers were a part of her upbringing, setting the stage for a life of cautious vigilance.
The first signs emerged during her freshman year of college, amidst a period of high stress. It started with severe abdominal pain, a symptom that prompted her to suspect porphyria given her family background. However, she was initially told she was too young for such an attack. The pain subsided temporarily, only to return with devastating force the following month, bringing relentless vomiting and an inability to tolerate food or water.
“I was often met with skepticism when requesting specific pain management, being wrongly labeled as ‘drug-seeking.’”
-Savanna, AIP patient.
Seeking help at a campus clinic proved futile; her concerns were dismissed as a common digestive issue. As her condition deteriorated over several days, severe dehydration finally led her to an urgent care facility, which immediately directed her to the Emergency Room. There, her mother became a crucial advocate, insisting on the specific testing for porphyria. What followed was a harrowing blur of pain, confusion, and metabolic disturbance that resulted in her admission to the Intensive Care Unit. Her memories of that first major attack are fragmented, fading in the ER and resuming days later in the disorienting environment of the ICU.
While the diagnosis confirmed AIP, it marked the beginning of a prolonged struggle. For the next three years, she endured monthly attacks, frequently linked to her hormonal cycle. Each hospitalization presented a new challenge in being believed. Without visible markers for her severe pain on standard tests and given her young age, she often faced skepticism regarding her pain management needs, at times being wrongly labeled. She learned to carry a detailed folder containing her official diagnosis and a standard treatment plan from a major clinic, a tangible tool to bridge the gap in understanding during crises.
Her original academic path in a demanding arts program became untenable as her health declined. When accommodations were revoked, the added stress exacerbated her condition. It was during a prolonged hospital stay that a new direction emerged. Finding solace and interest in understanding her own medical care, she engaged deeply with her treatment team. Encouraged by a compassionate specialist who reassured her that changing paths was not a failure, she made a pivotal decision. She left her initial majors behind and entered nursing school, driven by a desire to use her personal experience to foster empathy in patient care.
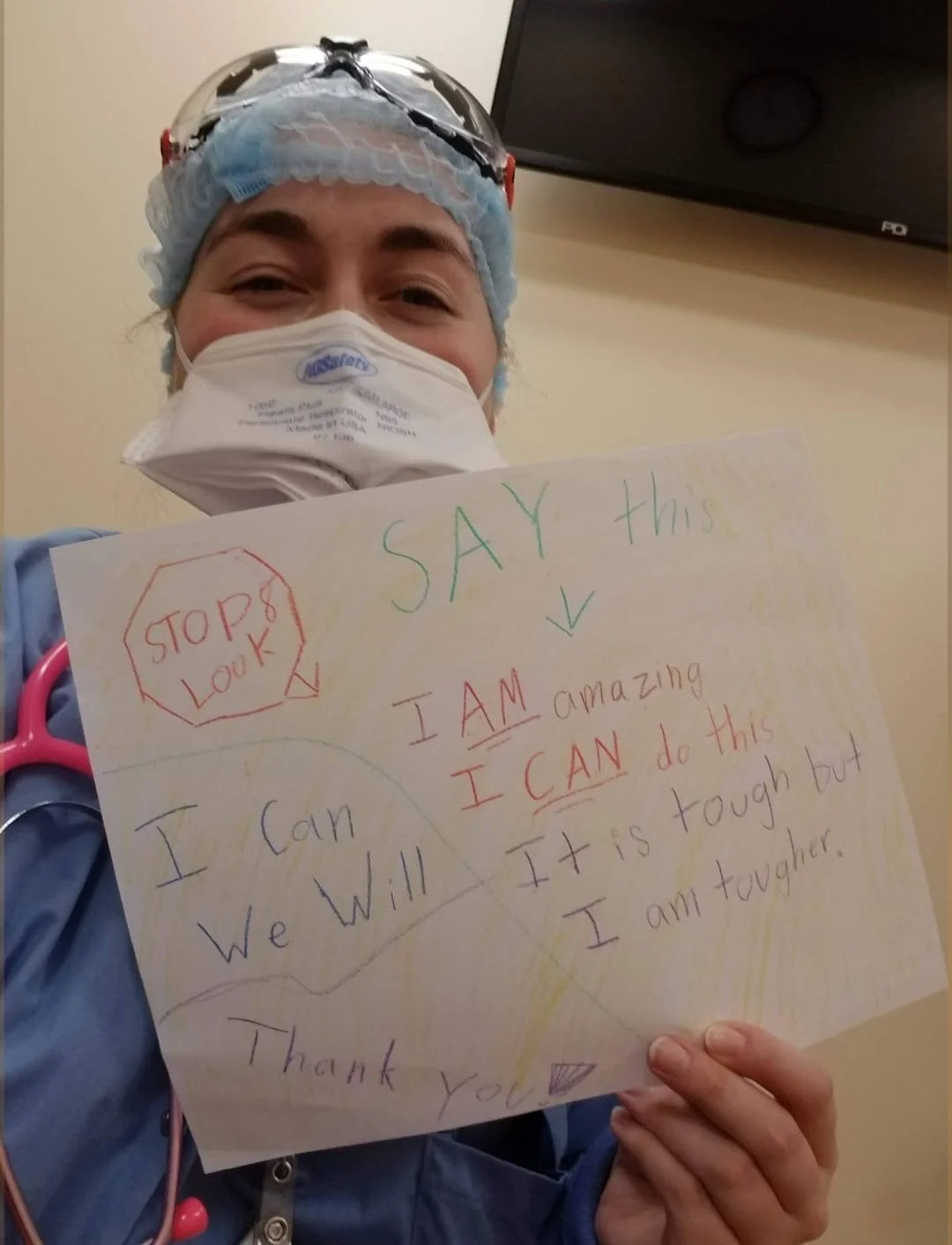
Savanna, now as a nurse.
Managing the condition involved a difficult process of trial and error. She received regular prophylactic treatments that, due to a lack of widespread familiarity with the protocol among providers, were often administered in ways that caused significant damage to her peripheral veins over time. Attempts at hormonal management initially provided relief but led to serious complications, including a life-threatening hemorrhage that required emergency intervention. For years, a low-dose hormonal device offered fragile stability, allowing her to manage chronic symptoms and ultimately complete her nursing degree.
A significant turning point came several years later when, through her own dedicated research as a nurse, she discovered a newly approved targeted therapy. She presented the information to her specialist, and together they decided to try it. This treatment, combined with the existing hormonal strategy, finally brought substantial and sustained relief. Recently, having achieved remarkable stability, she made the decision to remove the hormonal device, relying solely on the new therapy, a milestone that once seemed an impossible dream.
“More than anything, I wish for greater awareness.
For those in the medical field, I wish for the understanding that even if you cannot see the source of our pain, you can choose to believe us.”
Savanna holding a list of motivational phrases.
Her advice to those newly diagnosed centers on self-advocacy and preparation. She emphasizes the importance of becoming knowledgeable about one's own condition and assembling a physical portfolio containing the diagnosis, a typical treatment protocol, and a letter from a specialist. This packet serves as a critical voice during moments when the patient is too ill to articulate their needs, providing both credibility and a clear roadmap for emergency providers. She also stresses the importance of considering long-term venous access if recommended, to preserve one's physical resources for the future.
Above all, she wishes for greater awareness. For healthcare professionals, she hopes for a fundamental understanding that believing a patient's report of pain, even in the absence of visible proof, can fundamentally alter the care experience from one of trauma to one of compassion. Her journey stands as a testament to resilience, the power of self-education, and the ongoing need for empathy in medicine.
Savanna’s inspiring story.
Want to share your story? Contact us at katri@porphyria.org